Familial Cancer Testing – Specialist Pathway
Well-known familial cancer syndromes include hereditary breast and ovarian cancer (HBOC) syndrome and Lynch syndrome. For HBOC, a number of high and moderate risk genes that have been demonstrated to increase risk of breast and/or ovarian cancer can be tested. Testing of genes associated with Lynch and familial adenomatous polyposis (FAP) syndromes can also be important in the setting of inherited colorectal cancer.
Testing to detect genetic variants in the BRCA1 and BRCA2 genes is also used to determine eligibility for olaparib therapy in some patients with ovarian, breast or prostate cancer.
The new BraOVO Plus gene panel is important for breast cancer patients with a family history that includes ovarian cancer and is also useful for families where there is a mixed cancer picture of breast +/- ovarian +/- colorectal cancer.
Hereditary Breast, Ovarian & Prostate Cancer Tests
$449*
BraOVO Gene Panel
Results available within 3 – 4 weeks
$575*
BraOVO PLUS Gene panel
Results available within 3 – 4 weeks
$449*
BRCA1 & BRCA2
Results available within 3 – 4 weeks
$300*
Familial Cancer
gene testing (single)
- Single gene testing for known family pathogenic variant
- MBS Item 73297
- Select genes only covered
Results available within 3 – 8 weeks
Familial Colorectal Cancer Tests
* When MBS criteria are not fulfilled.
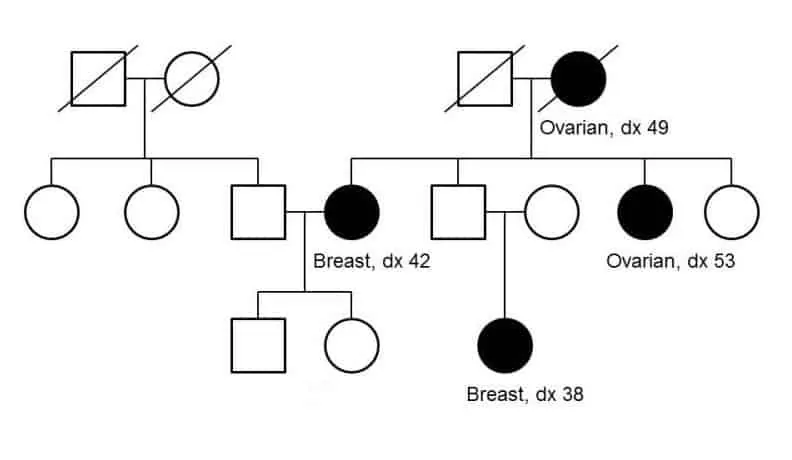
Some families may have an increased risk of developing certain types of cancer through the inheritance of variants (mutations) in certain genes. Testing for these genetic variants can determine whether a patient might be at increased risk of developing cancer and suggest an appropriate prevention or surveillance strategy. This test is Medicare eligible for those patients satisfying testing criteria.
There are now Medicare rebates available for testing in women with breast and ovarian cancer who are at high (>10%) risk for detecting a genetic cause. Please refer to the HBOC Risk calculators section below for more information.
| Test Name | Breast/Ovarian Cancer BRaOVO Gene Panel | |
|---|---|---|
| Clinical Indication | Used to: 1. Determine presence of pathogenic variations in patients with a personal and/or family history suggestive of high risk (>10%) of having Hereditary Breast and Ovarian Cancer Syndrome. 2. Determine presence of pathogenic variations in patients with a biological relative with a confirmed pathogenic variation in one or more of the genes specified below | |
| Gene(s) | ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, PALB2, PTEN, RAD51C, RAD51D, STK11, TP53 | |
| Method | Massively Parallel Sequencing | |
| Turn Around Time | 3 – 4 weeks | |
| Medicare Eligibility | 73296 – criteria apply | |
| Sample Type | Blood x 2 | |
| Collection Type | 10mL EDTA tube | |
| Special Instructions | 2 x Bloods taken at 10 minute intervals. Pre test genetic counselling required. Patient to sign consent form prior to testing. | |
This panel is important for breast cancer patients with a family history that includes ovarian cancer and is also useful for families where there is a mixed cancer picture of breast +/- ovarian +/- colorectal cancer.
| Test Name | BraOVO Plus Cancer Gene Panel |
|---|---|
| Clinical Indication | Used to: 1. Determine risk for patients with a personal and/or family history suggestive of Hereditary Breast and Ovarian Cancer Syndrome. |
| Gene(s) | ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, PALB2, PTEN, RAD51C, RAD51D, STK11, TP53, MLH1, MSH2, MSH6, PMS2, EPCAM |
| Method | Massively Parallel Sequencing |
| Turn around time | 4 weeks |
| Medicare Eligibility | 73296 – conditions apply |
| Sample Type | Blood x 2 |
| Collection Type | 10mL EDTA tube |
| Special Instructions | 2 x Bloods taken at 10 minute intervals. Pre test genetic counselling required. Patient to sign consent form prior to testing. |
Hereditary cancers are those where altered genes contribute to an inherited predisposition to certain cancers. In breast cancer, 5-10% are due to inherited genetic alterations. These are most commonly identified in the breast cancer susceptibility genes, BRCA1 and BRCA2, but can also occur in other genes.
BRCA status can have significant implications for the therapeutic management of carriers. Cancer is complex, as one gene may be responsible for many different cancer types or many genes acting together may increase a woman’s risk of developing breast and ovarian cancer. Therefore, it is recommended these tests be ordered by, or in consultation with, specialists familiar with the implications for management.
Testing for genetic variants in BRCA1 and BRCA2 can also be used to determine eligibility for olaparib maintenance therapy in relapsed high grade serous ovarian cancer, metastatic castration-resistant prostate cancer, triple negative early breast cancer, or hormone receptor positive, HER2-ngative, early breast cancer with a high-risk characteristic.
| Test Name | BRCA1 and BRCA2 Genetic Testing |
|---|---|
| Clinical Indication | Used to: 1. Determine eligibility for treatment with olaparib under the PBS in patients with relapsed high grade serous ovarian cancer or metastatic castration-resistant prostate cancer. 2. Determine eligibility for treatment with olaparib under the PBS in patients with triple negative early breast cancer; or hormone receptor positive, HER2-negative, early breast cancer with at least one of the following high-risk characteristics:
|
| Gene(s) | BRCA1, BRCA2 |
| Method | Massively Parallel Sequencing |
| Turn around time | 4 weeks |
| Medicare Eligibility | 73295 – conditions apply 73304 – conditions apply |
| Sample Type | Blood x 2 |
| Collection Type | 10mL EDTA tube |
| Special Instructions | 2 x Bloods taken at 10 minute intervals. Pre test genetic counselling required. Patient to sign consent form prior to testing. |
Risk prediction models can be used to calculate the likelihood of carrying a variant in selected cancer risk genes. These are evidence-based tools that can assist in determining whether genomic testing should be performed.
The models available for HBOC are:
Manchester Score – from St Mary’s Hospital in Manchester.
BOADICEA – from Cambridge University – canrisk.org
Penn II Risk Model – from the University of Pennsylvania – pennmodel2.pmacs.upenn.edu/penn2
| Test Name | Predictive familial cancer test |
|---|---|
| Clinical Indication | Determine presence of mutations in patients with a biological relative with a confirmed pathogenic variation in one or more of the genes specified below. |
| Gene(s) | ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, PALB2, PTEN, RAD51C, RAD51D, STK11, TP53 |
| Method | Massively Parallel Sequencing |
| Turn around time | 2 weeks |
| Medicare Eligibility | 73297 – criteria apply and only particular genes covered. ATM, BARD1, BRIP1, CHEK2, RAD51C and RAD51D may be tested but are not rebatable. |
| Sample Type | Blood x 2 |
| Collection Type | 10mL EDTA tube |
| Special Instructions | 2 x Bloods taken at 10 minute intervals. Pre test genetic counselling required. Patient to sign consent form prior to testing. |
Colorectal cancer is the third most common type of newly diagnosed cancer in Australia. It is estimated that 30% of patients with colorectal cancer have a family history of the disease, and up to 10% have genomic variants associated with inherited cancer syndromes including Lynch syndrome (LS).
A diagnosis of LS is confirmed by the detection of a pathogenic germline variant in one of the MMR genes (MLH1, MSH2, MSH6 and PMS2) or the EPCAM gene.
| Test Name | Lynch Syndrome Gene Panel |
|---|---|
| Clinical Indication | Used for investigation of Lynch Syndrome in patients with colorectal cancer or endometrial cancer where there is a familial risk of ≥10%. |
| Gene(s) | MLH1, MSH2, MSH6, PMS2, EPCAM |
| Method | Massively Parallel Sequencing |
| Turn around time | 4 weeks |
| Medicare Eligibility | 73354 – conditions apply |
| Sample Type | Blood x 2 |
| Collection Type | 10mL EDTA tube |
| Special Instructions | 2 x Bloods taken at 10 minute intervals. Pre test genetic counselling required. Patient to sign consent form prior to testing. |
Guidelines recommend testing to confirm the diagnosis of an inherited CRC syndrome in a patient with a personal history of disease in the following circumstances:
- APC gene testing is indicated in patients with ≥10 colorectal adenomas before age 30, or ≥20 colorectal adenomas regardless of age.
- MUTYH gene testing is indicated for patients with ≥20 colorectal adenomas at any age, but could also be considered in patients with fewer polyps following review by a familial cancer service, and patients with an FAP phenotype but no identifiable APC variant.
| Test Name | FAP Gene Panel |
|---|---|
| Clinical Indication | Used for investigation of FAP/MAP in patients with adenomatous polyposis where there is a familial risk of ≥10%. |
| Gene(s) | APC, MUTYH |
| Method | Massively Parallel Sequencing |
| Turn around time | 4 weeks |
| Medicare Eligibility | 73355 – conditions apply |
| Sample Type | Blood x 2 |
| Collection Type | 10mL EDTA tube |
| Special Instructions | 2 x Bloods taken at 10 minute intervals. Pre test genetic counselling required. Patient to sign consent form prior to testing. |
| Test Name | Colorectal cancer predictive test |
|---|---|
| Clinical Indication | Determine presence of mutations in patients with a biological relative with a confirmed pathogenic variation in one or more of the genes specified below. |
| Gene(s) | MLH1, MSH2, MSH6, PMS2, EPCAM, APC, MUTYH |
| Method | Massively Parallel Sequencing |
| Turn around time | 2 weeks |
| Medicare Eligibility | 73357 – criteria apply |
| Sample Type | Blood x 2 |
| Collection Type | 10mL EDTA tube |
| Special Instructions | 2 x Bloods taken at 10 minute intervals. Pre test genetic counselling required. Patient to sign consent form prior to testing. |
Resources
Leading the way to improved health
results in the shortest turnaround time.